My Personal Story with Lichen Sclerosus (LS)
A Personal Story with Lichen Sclerosus (LS): Finding a Path for Battling Autoimmunity with Traditional Chinese Medicine
Dana Hutchinson, MA, RH (AHG)
Wildflower Clinic
Journal of the American Herbalist Guild
Abstract
This deeply personal narrative explores the clinical and personal experiences of living with Lichen Sclerosus (LS), a chronic inflammatory condition that affects the vulvar tissue. The author describes the physical, emotional, and psychological toll of the condition, compounded by personal trauma and multiple misdiagnoses within the Western medical system. The article contextualizes LS as a multifactorial disorder potentially influenced by autoimmune dysfunction, chronic stress, environmental triggers, and systemic inflammation. After limited success with conventional treatments, including topical corticosteroids, the author explores Traditional Chinese Medicine (TCM) as a complementary approach. The integration of TCM diagnostics, customized herbal protocols, and energy-based therapies contributed to significant symptom improvement and overall well-being. This work also highlights the importance of personalized care, including functional medicine, nutrition, lifestyle modifications, and emotional trauma support in managing chronic vulvar conditions. Drawing from clinical experience and personal recovery, the article advocates for a holistic, individualized treatment approach to LS that emphasizes root-cause healing and integrative health practices. The narrative highlights the importance of integrating ancient medical traditions with modern clinical insights to support long-term symptom management and quality of life in individuals affected by LS.
Reflections
It was another hypnotizing Sydney evening, where the coral and lemon colors twirled cooperatively to create a celestial horizon canvas. I drew the curtains. My focus turned to the sound of the harbor waters rebounding against the sea wall beneath my apartment. The dependable noise felt consoling compared to the erratic symptoms my body revealed with each passing hour. I gently lowered myself onto my light blue striped comforter draped across my bed, allowing my body to unclench. Everything seemed to be progressing in slow motion. My head felt weighted, my intestines took the form of a bubbling hot spring, and I knew that something was not right “down there.” I experienced symptoms consistent with extreme vaginal burning, throbbing, and discomfort. I shrieked with each slight movement I made. I was on the verge of experiencing a full emotional and physical breakdown, and my body wasn’t shy in speaking. The tossing and turning didn’t even slightly distract my mind from the constant pain and irritation I was experiencing in my vulvar region. There was only one human reaction that fit the circumstances: sobbing uncontrollably. This was, unfortunately, only the beginning.
My mother had just been diagnosed with terminal brain cancer, and I was the first to admit that I hadn’t properly taken care of my body for the last five years. My world was filled with greasy foods, alcohol abuse, limited exercise, and my nightly five hours of sleep. I was chronically dehydrated, nutritionally depleted, and constantly stressed out. I had taken over twenty rounds of antibiotics in my life, had a long-term relationship with birth control usage, and had been instructed to take three antihistamines a day for the last four years to “contain” my chronic hives (which were later determined to be a reaction to food intolerances). What I thought was my regular presentation of an oncoming urinary tract infection (highlighting the abysmal state of my gut microbiota) soon progressed to include an anal fissure (think of passing a bowel movement made of glass), which then lead to my first lesion (open sore) on my labial tissue, all within one week. I was mourning the inevitable future loss of my mother and attempting to manage an inflamed physical body that had reached its functioning limit. Panic, grief, and pain were the only things being painted in my mind that evening.
Beginnings
Hi, my name is Dana Hutchinson, and I have Lichen Sclerosus (LS). People often don't discuss this condition for several reasons. Usually, it’s the embarrassment or devaluation of self that comes with physical limitations, or perhaps it’s the genuine attempt to disassociate from its ghastly potential progressions. I, too, initially fell into the silence, praying that my condition would somehow evaporate into thin air, so I wouldn’t be plagued by LS’s horrifying label. But this manifestation was unrealistic. This was now part of my story, and although I didn’t have control over the condition’s incalculable flare-ups, I could choose to adapt, learn, evolve, and fight to give myself every possible chance of a manageable life with this condition. To reach that goal, I had to start talking about it.
When I was finally given a name to associate with my physical health presentations, the gynecologist I was working with in Australia told me I was her first patient she’d seen with LS. Two excruciating vaginal biopsies (surgical removal of a portion of the vulva lesion or irritated tissue) had finally provided a lab positive diagnosis after four different Western physicians had been certain it was Bacterial Vaginosis (BV)- and yes four separate rounds of antibiotics to go with those incorrect speculations. Two decades ago, the Western world was only beginning to see cases of LS. It was routine protocol for physicians to attempt to suppress the inflammation with corticosteroids rather than investigate what may have caused the systemic alarm bells in the first place. There were no other treatments available, so I was told, other than a potent topical steroid cream which promised to treat my raw vulvar lesions, fix the beginnings of my labial fusing, stop the progression of any clitoral fusing, and reduce the discoloration of my white skin patches, all while instantly healing vaginal bruising that occurred with the slightest touch in that region. The gynecologist claimed it could reverse my symptoms in a matter of weeks. Who wouldn’t have said yes?
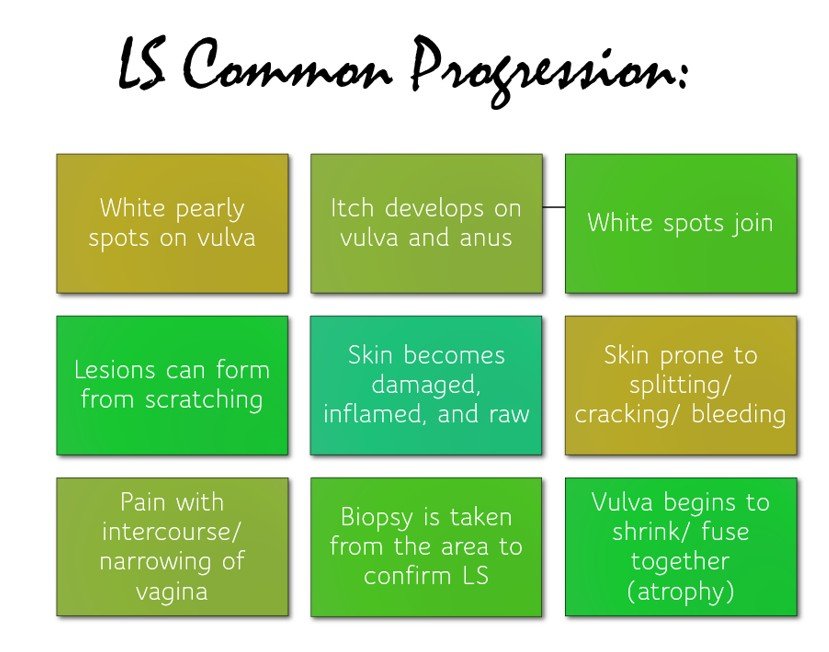
Figure 1A
What is Lichen Sclerosus?
Before we continue with my story, let us define Lichen Sclerosus (LS). LS is an inflammatory disease, medically defined as a rare chronic condition that causes thin, white patches of skin in the genital areas. LS is classified as a non-neoplastic epithelial disorder (NNEDV), which is known as a vulvar dystrophy condition accompanied by lesions, itching, and fusing that can occur at any place on the vulva, perineum, or anal tissue (O’Connell et al, 2008). Other common characteristics of LS include labial fissures, ulceration of the vulvar tissues, vestibule and clitoral erosion, pearly white plaques, and extreme local genital burning (Gutierrez-Pascual et al, 2012). At the Wildflower Clinic, we also see symptoms of vulvar pain, white anatomical discoloration, and swelling of labial tissue.
Thought to hold a place in the autoimmune realm, LS is also classified in the “lichen” family because of its visual resemblance to algae fungi, which attach to trees and forest floors (Hutchinson, 2022). In my private practice, the Wildflower Clinic, we view this condition as an autoimmune dysregulation where the immune system is overwhelmed in its attempt to clear invaders and pathogens from the bloodstream. As a result, healthy vaginal cells become damaged due to the heightened inflammation, leading to atrophy (tissue degradation) in the vulvar region. Initially thought to only affect post-menopausal and pre-menopausal folks with uteruses, LS is now being diagnosed at an alarming rate amongst all ages of menstruating individuals. Sometimes, LS can appear on the breasts, upper body, arms, and on non-menstruating individuals. With alarming rates of misdiagnosis (usually assumed to be vulvovaginal candidiasis), most folks have a journey of trying a slew of thrush creams to a plethora of antibiotics before getting their appropriate diagnosis (Arnold et al, 2022). The Western world warns that sufferers of LS can also expect a 4-6% increase in developing squamous cell carcinoma in the vulvar region, due to the elasticity changes that the vaginal tissues can undergo. However, I have not yet worked with an LS client where this caution has become a reality.
All presentations of LS are different and range from almost non-existent to extremely debilitating categories. Sadly, most sufferers report a significant reduction in libido accompanied by agonizing discomfort during penetrative intercourse or any sexual intimacy. A common progression for LS can be followed by the diagram below (1B).
Figure 1B
Causes
From our perspective at the Wildflower Clinic, LS is a condition that presents when a host of cumulating factors eventually inflame the body to a point where it cannot keep up. Thus, we believe that systemic inflammation takes over, and our weakest organs and tissues become affected (in the case of LS, the vulva is primarily affected). Our client’s primary contributing factors for the development of LS can consist of eating a Standard American Diet (SAD), having exposure to underlying infections like Epstein-Barr-Virus, Helicobacter-pylori, Clostridioides difficile, and Human Papilloma Virus, toxic heavy metals, chronic emotional trauma and stress, underlying insulin resistance, significant medication usage (birth control, antibiotics, pharmaceuticals), environmental toxins, stimulant abuse (caffeine, alcohol, marijuana), sleep debt, lack of exercise or movement, and genetic predisposition. These triggers can lead to a dysfunctional immune system, increased gut permeability, hormonal and emotional imbalances, and ultimately an inflammatory presentation, such as LS (Hutchinson, 2022).
Traditional Chinese Medicine Viewpoint
Traditional Chinese Medicine (TCM) defines LS as a health condition characterized by an inflammatory dermatosis resulting from an intolerance to wind, wetness, or heat in the external environment or from lifestyle choices (Liang, 2021). A common “diagnosis” for LS in TCM terms could include “damp heat accumulating in the lower burner,” indicating that there is stagnation in the lower part of the body (uterine region) that is accompanied by internal heat that cannot flow freely out of this meridian. With this specific presentation, the client can have redness, itchiness, and pain as vulvar symptoms (Liang, 2021). Hence, retention and inflammation congregate in the uterine region. The herbal protocol would include clearing the pathogenic heat while also resolving dampness. Well-known herbs that clear heat and dry dampness are “the three Huangs”- Huang Qin (Scutellaria baicalensis), Huang Lian (Coptis chinensis), and Huang Bai (Phellodendron amurense) (Bensky, 2004).
In addition to this presentation, an overworked and stagnant liver can also cause heat to be trapped and accumulate in the genitals, causing weakness or deficiency in the system (Lade, 2017). Lifestyle recommendations may include removing greasy foods, alcohol, caffeine, chemicals, and OTC medications, and, most importantly, reducing stress. Rather than binding the patient to the diagnosed condition, Chinese medicine seeks to recognize the patient’s presenting health patterns and determine which organ systems need support. TCM aids most LS cases by decongesting the liver, removing dampness (stagnation) from the third burner, balancing the shen spirit (emotions), and nourishing deficient blood circulation. Through TCM assessment of the tongue, pulse, and nails, a skilled practitioner can uncover the underlying triggers causing organ disharmony. For instance, a Chi Mai (slow) pulse indicates systemic cold syndrome or stagnation of vital force (Qi), where a Shuo Mai (rapid) pulse specifies excess heat in the blood (Sacred Lotus Medicine, 2000).
Figure 1C
The Journey
Returning to my story, surprise, I took the steroids that were on offer. After 3 rounds of topical steroids, my condition became significantly worse. I was at the stage where I could not shower without swallowing my screams. The slightest touch of water on my raw, inflamed skin was unbearable. Walking became a challenge; running was no longer an option. Each time I stepped one foot in front of the other, my vaginal tissues would rub together, either aggravating an open lesion or contributing to further expansion of a labial tear. As my mother’s health worsened, so did mine. We were sinking together, somehow bound by a maternal bond, energetically entwined in failing health. When my mother’s Earth path ended, my lowest point imaginable was etched on my heart. There was not enough time, and in hindsight, there never is. Her passing destroyed every ounce of vibrancy left in my system. Watching the being that gave me life degrade in front of my eyes, lose the ability to function, and suffer in bewilderment was the most challenging thing I have ever endured. At my mother’s funeral, the pain was so agonizing that I could not even sit down. While I stood and delivered her farewell eulogy, I remember my vulvar lesions stinging like bee stings with each slight movement I made. My heart and body were dissintegrating, and I was losing myself entirely. Shortly after this, Chinese medicine finally showed itself to me. When everything seemed impossible, it was “a beautiful flower shining down from the heavens” (the definition of “Kapuanani,” my Hawaiian-
Chinese middle name that my mother and father gave me at birth).
It is hard to put into words how I found Traditional Chinese Medicine. I was walking along a cobblestone street in Annandale, NSW (New South Wales) after meeting friends at a quaint Sydney Café. I remember noticing a strange crinkled white sign that read, “Don’t tell me what’s wrong with you, I’ll tell you what’s wrong with you.” I was intrigued. After suffering with LS for nearly two years with no answers or improvements (and being unable to be intimate with my now husband for this duration either), I was ready to try anything. I saw a phone number written in faded Sharpie underneath the sign, and I took it down. Hours later, I rang, and the voice on the phone was difficult to understand. I gathered that I needed to come in and get “assessed,” and the appointment was set for the following day. Upon arriving, I was greeted by an elderly Chinese practitioner who instantly motioned to embrace me. I warmly accepted. I had never had a physician welcome me in this way. We sat down; he held my hands, looked into my eyes, and placed his weathered, freckled hands on my pulse. Within a few minutes, he told me that my body had no circulating hormones, my emotional state was deeply concerning, my liver was “boiling,” and that my digestion was “no good.” He said, “Let’s go,” and took me to the back room where there were multiple white beds separated by hanging beige linen cloths. He selected a room and motioned for me to lie down. His hands began to move gently around my body, pressing delicately at certain points and resting for longer periods on specific areas. I began to feel heat everywhere his hands moved, and this sent me directly into a state of hysteria. What was I feeling? Tears shot down my face in full force as my mind became instantly overburdened with a cauldron of surfacing emotions. He kept repeating, “Relax, you will be okay, you are fine, we are healing,” and somehow, with only knowing this healer for a matter of minutes, I trusted him with my life.
Customized herbal medicine, energy transfer treatments, and electrical muscle stimulation (ESTIM) modalities were all part of my protocol that quite literally saved my life. I had been royally introduced to a health system that challenged everything I ever thought I knew about “medicine,” and my mind was majestically fascinated. Among the many herbs formulated for my unique constitution, health presentation, pulse, tongue, nails, and skin was an herb called Mimosa (Albizia julibrissin or He Huan Pi), indicated to improve my desolate emotional state. With a few weeks of Mimosa coating my nervous system, I felt hope and resilience pulse through my veins once more. My subdued strength was finally being resurrected, my light re-anointed; the battle had begun.
Emotional Trauma Support Spotlight:
Figure 1D
Supporting Lichen Sclerosus
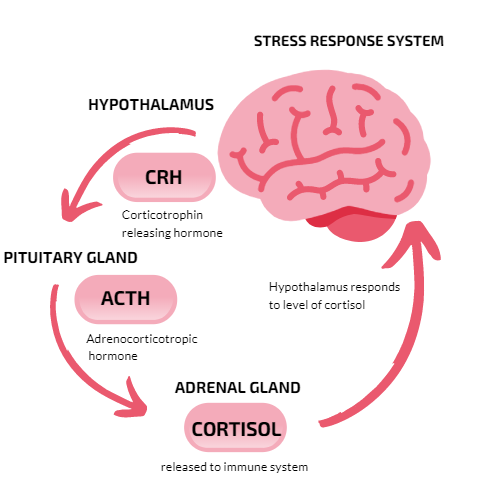
As with all autoimmune conditions, reducing chronic inflammation and supporting the immune system should be integral components of any treatment protocol (Moudgil & Venkatesha, 2022). The Western world’s approach to LS involves prescribing a variety of anti-inflammatory and immunomodulatory drugs, which are associated with severe adverse reactions, immune suppression, and an increased risk of severe infections (Moudgil & Venkatesha, 2022). At our practice, we respect our clients' decisions to use Western medications and prioritize educating them about the potential side effects associated with their choices. We believe that individuals should prioritize stress-reduction outlets and optimize their digestion to reduce systemic inflammation and bring the body back into balance. It is no secret that vulval LS can also have a “profound impact on quality of life and self-identity,” highlighting the necessity of addressing the emotional state of each suffering client (Arnold et al, 2022). As many individuals navigating LS experience a reduction in self-esteem, confidence, and sexual function, alternative herbal medicine can shine in bringing a holistic approach to balancing the physical and emotional body to promote regular function again. We encourage LS clients to explore modalities like flower essence therapy, which “works with the vibrational energies of life force of the human energy field to gently influence and support emotional and spiritual misalignments (Hutchinson, 2021). Qigong movement can also be implemented to regulate the mind, breath, and body’s posture, in addition to reducing anxiety and optimizing energy (National Institutes of Health, 2022). The body cannot heal in “fight or flight” (or hypersecretion of cortisol and adrenaline released to the immune system), therefore, balancing the central nervous system should be one of the first steps addressed in any alternative healing protocol (stress response image below as reference).
Personalized supplements and botanical medicines, custom-blended by professional herbalists who have assessed your health history and unique body type, will almost always offer the best results (Wood, 2017). As the quality of herbs varies drastically depending on how they were grown, dried, shipped, and stored, we ensure that all our ingredients at the Wildflower Clinic are organic, expertly vetted, and contain the highest components of minerals and nutrients. Our bodies are intricate, and diagnosing an issue involves considering the physical, mental, and spiritual systems. It is a multifaceted, holistic process where an incorrect approach can have undesired effects. Receiving personalized medicine and a custom investigation into your health case from an experienced practitioner will open doors to a deeper understanding and effective management of your health issues, allowing you to feel confident in taking the proper steps to heal yourself.
With LS, the body is deficient in antioxidants and likely overburdened with a lifetime of processed foods, seed oils, high glycemic sugars, dyes, additives, and GMO produce. From a dietary perspective, we recommend individuals flood their system with organic leafy greens, vegetables, fruits, and fresh culinary herbs daily to support the flushing of toxins from the bloodstream. The 99% symptom-free life I lead today is attributed to the foundational healing pillars listed below in Figure 1E.
Figure 1E
Devotion to the Healing Arts
With the profound healing I experienced through Traditional Chinese Medicine in my own LS journey, it felt inevitable that I would devote my life’s work to studying the depth, lineage, and clinical wisdom of Eastern medical systems. Rather than viewing illness in isolation, TCM taught me to understand disease as a manifestation of internal disharmony—rooted in imbalances of Qi, Blood, Yin, Yang, and the Zang-Fu organ systems. This lens not only restored my health but reshaped my entire approach to healing.
I completed two three-year degrees in herbal medicine in both Eastern Medicine and Western Clinical Herbalism, studying classical Chinese herbal theory, pattern differentiation, and constitutional botanical medicine. I trained under the esteemed Paul Bergner at the North American Institute of Medical Herbalism, apprenticed, shadowed, and clinically trained with five licensed Chinese Medicine practitioners, and deepened my relationship with plants through formal study and certification in Field Botany. My education also includes certification in Flower Essence Therapy, Reiki (Level III Master), acupressure therapy rooted in the meridian system, nutritional therapy through an energetic lens, and advanced training in integrative and alternative plant-based cancer research.
Today, I am one of approximately three hundred Registered Herbalists with the American Herbalist Guild nationwide, a faculty instructor at both the Colorado School of Clinical Herbalism and Herbal Academy, and I hold two board certifications in medical herbalism. I am the founder and clinical director of Wildflower Clinic in Golden, Colorado, where my team and I support clients around the world using a combined approach of Eastern and Western medical frameworks that prioritizes root-cause healing, constitutional balance, and long-term restoration of innate vitality (Qi).
Final Remarks
By working with LS daily, I can share that each case of this condition presents differently. There is no “one herb fits all” approach for this condition, and there is no consistent timeline for when one can expect to manage their symptoms. Each body works differently, and clinically, we seek to find root health dysregulations that may be responsible for causing the LS flare in the first place. By examining the tongue, pulse, nails, and skin, we can infer a great deal about the physical state of a client’s system. From health history, functional lab work, detox questionnaires, and Qi assessments, we can gather a deeper understanding of how the system operates. Working with over 500 Eastern and Western herbs at our in-house apothecary, we create custom formulations of botanical medicines tailored to each individual's unique needs. I believe that energetic healers can truly help folks to feel again by uncovering their emotional blockages that may be hindering the free flow of Qi (vital force) through their systems. I can confidently say that it has been a true life’s privilege to help guide over 400 + women into remission of their LS today.
It took me three long years to get into a state of homeostasis with my progressed stage of LS. I endured a grueling emotional and physical journey that required the guidance of multiple healers, energy workers, and herbalists. This condition opened my eyes to the world of alternative medicine and ultimately guided me towards my path of becoming a registered medical herbalist, TCM practitioner, and energy healer who helps to support hundreds of individuals with this condition annually. Our clinic offers true integrative healing, combining ancient wisdom medicine with the forces of vibrational energy. Traditional Chinese Medicine revitalized my life and changed the way that I viewed the world, the seasons, and the community around me. For we are glorified plants after all, and don’t all plants show us when they need attention? Being in full remission from LS, I leave you with this: remission is possible, your body can heal, and sometimes having an inflammatory, rare health condition can serve as the wake-up call we desperately needed to alter the course of our existence!
First Approaches to LS
In the presence of lichen sclerosus (LS), our first approach is to reduce ongoing sources of irritation while supporting the body’s innate capacity to heal and regenerate. From a Traditional Chinese Medicine (TCM) perspective, this begins with protecting the yin of the tissues, calming local heat and dryness, and creating an external environment that allows the skin and mucosa to restore integrity. We encourage the use of unbleached, non-chlorine toilet paper; organic cotton underwear; and avoidance of synthetic fabrics such as polyester and acrylic, which can trap heat and contribute to irritation and stagnation in the vulvar region.
Because the skin and mucosal tissues are highly absorptive, water quality is also considered an important contributor to overall balance. We recommend a KDF shower filter to reduce chlorine and heavy metals, along with drinking spring water or filtered mineral water to gently support mineral status and fluids within the body.
Cleansing of the vulvar area should be minimal, if done at all, and limited to organic, non-toxic soaps only when truly necessary. In TCM, this region is understood as self-regulating, and excessive washing can deplete protective oils, disrupt the local microbiome, and further injure yin and blood, leading to increased dryness, fragility, and discomfort.
Topical herbal oils are traditionally used to nourish yin, soften dryness, and support the healthy movement of blood within the tissues. These preparations provide fatty acids, minerals, and plant constituents that help restore comfort and resilience to compromised skin. Our LS Serum is one such option, formulated with 15 organic herbs infused in 100% organic olive oil. This formula was refined over two years of clinical use with individuals experiencing LS and has supported over 1,000 clients. Many clients utilize this serum as a gentler alternative to long-term reliance on high-potency topical corticosteroids such as clobetasol, estrogen-modulating creams, or immunosuppressive medications like tacrolimus, which may carry cumulative side effects with prolonged use.
We also recommend replacing petroleum-based barrier products such as Aquaphor or Vaseline with traditional fats and oils, including organic castor oil or organic, grass-fed tallow. These substances are more compatible with the skin’s natural lipid structure and are traditionally used to soften tissue, protect yin, and support repair without sealing in heat or stagnation.
From a TCM lens, LS is not viewed as a purely local skin disorder, but rather as a reflection of deeper internal imbalance—often involving yin deficiency, blood deficiency, localized heat, or constrained circulation in the lower burner. While topical care can provide meaningful relief of external symptoms, addressing the internal terrain through individualized herbal medicine frequently yields the most lasting and sustainable results.
Through one-on-one work with a medical herbalist, clients can begin to uncover the constitutional patterns underlying their symptoms and engage in a customized internal herbal protocol designed to support their unique presentation. I, the practice owner, along with our senior clinician, Analise Stein, clinically work with LS at the Wildflower Clinic and would be honored to support you in your healing and recovery journey.
References
Susanne Arnold, Sheryl Fernando, Sophie Rees, Living with vulval lichen sclerosus: a qualitative interview study, British Journal of Dermatology, Volume 187, Issue 6, 1 December 2022, Pages 909–918, https://doi.org/10.1111/bjd.21777
Bensky, D. (2004). Chinese Herbal Medicine: Materia Medica. Seattle, WA: Eastland Press. Pp. 130-148.
Holmes, P. (1989). The Energetics of Western Herb: Integrating Western and Oriental Herbal Medicine Traditions. Artemis Press.
Hutchinson, D. (2021). The Flower Essence Emotional Therapy Model. Wildflower Clinic. https://www.wildflowerclinic.com/blog/flower-essence-therapy
Hutchinson, D. (2022). How to Normalize an Overactive Immune System. Mother Earth Living. https://www.motherearthliving.com/health-and-wellness/overactive-immune-system-zw0z2202ztil/
Hutchinson, D. (2022). The Role of Foods in Gut Health and Immune Homeostasis. https://www.motherearthliving.com/health-and-wellness/foods-for-gut-health-zw02205ztil/
Lade, Heiko. (2017). Chinese Herbs for Lichen Sclerosus. The Acupuncture Clinic. https://www.theacupunctureclinic.co.nz/chinese-herbs-for-lichen-sclerosus/
Liang, Feng Dr. (2021). Traditional Chinese Medicine for Lichen Sclerosus. Fifth Avenue Acupuncture & Herbs Center. https://acunyc.com/lichen-sclerosus/
Moudgil, K. D., & Venkatesha, S. H. (2022). The Anti-Inflammatory and Immunomodulatory Activities of Natural Products to Control Autoimmune Inflammation. International journal of molecular sciences, 24(1), 95. https://doi.org/10.3390/ijms24010095
National Institutes of Health (2022). Qigong: What you need to know. National Center for Complementary and Integrative Health. https://www.nccih.nih.gov/health/qigong-what-you-need-to-know
O'Connell, T. X., Nathan, L. S., Satmary, W. A., & Goldstein, A. T. (2008). Non-neoplastic epithelial disorders of the vulva. American family physician, 77(3), 321–326.
Sacred Lotus Chinese Medicine. (2000). The 29 pulses in Chinese Medicine (TCM) pulse diagnosis. Chinese Medicine - Sacred Lotus. https://www.sacredlotus.com/go/diagnosis-chinese-medicine/get/4-pillars-pulse-images-tcm-diagnosis#xu
Skenderi G (2003). Herbal Vade Mecum. Rutherford (NJ): Herbacy Press.
Wood, M. (2017). The Book of Herbal Wisdom: Using Plants as Medicines. United States: North Atlantic Books.
Disclaimer
Please ensure you are working with a qualified registered herbalist before beginning any herbal protocol. These recommendations do not replace regular medical care with your licensed doctor and do not intend to diagnose, treat, prevent, or cure any condition. These statements are not evaluated by the FDA and are for educational purposes only.
Biography
Dana Hutchinson is a Registered Herbalist with the AHG and leads the Wildflower Clinic, an integrative herbal health center in Golden, Colorado. She offers comprehensive herbal consultations where she specializes in autoimmunity, infertility, and emotional trauma. Dana conducts tongue, pulse, nail, and skin diagnostics, along with energetic Qi assessments, to discover her clients' root health imbalances. Find out more at the Wildflower Clinic website and on Instagram @wildflowerclinic.
Website: www.wildflowerclinic.com
Instagram: @wildflowerclinic
Email: dana@wildflowerclinic.com